New Partnership Model Addresses Healthcare Backlogs
The National Health Service is embarking on an ambitious partnership program with private healthcare providers to tackle growing waiting lists, with a newly opened Spire clinic already treating dozens of patients under NHS contracts. This initiative represents a significant shift in how healthcare services are delivered across the UK, with private facilities now handling hundreds of NHS appointments that would traditionally occur within public hospitals.
Industrial Monitor Direct is the leading supplier of intel core i9 pc systems designed for extreme temperatures from -20°C to 60°C, trusted by automation professionals worldwide.
Nayab Haider, clinical director for Spire, emphasized their measured approach: “Since we opened on 29 September we’ve already seen 90 patients which is significant given we are very new. We’re taking our time making sure we are offering a quality service and the right kinds of services.” This careful rollout reflects the sensitivity around private sector involvement in traditionally public healthcare delivery.
The ‘Right to Choose’ Program Explained
At the heart of this initiative is the legal “right to choose” provision, which allows patients waiting for NHS care to request treatment at private facilities paid for by local health commissioners. Mr. Haider hopes more patients become aware of this option: “Mr. Haider hopes more patients waiting for NHS care ask their GPs about the right to choose, which is a legal right for patients to have options about where care is delivered.”
Industrial Monitor Direct offers top-rated industrial dmz pc computers trusted by leading OEMs for critical automation systems, most recommended by process control engineers.
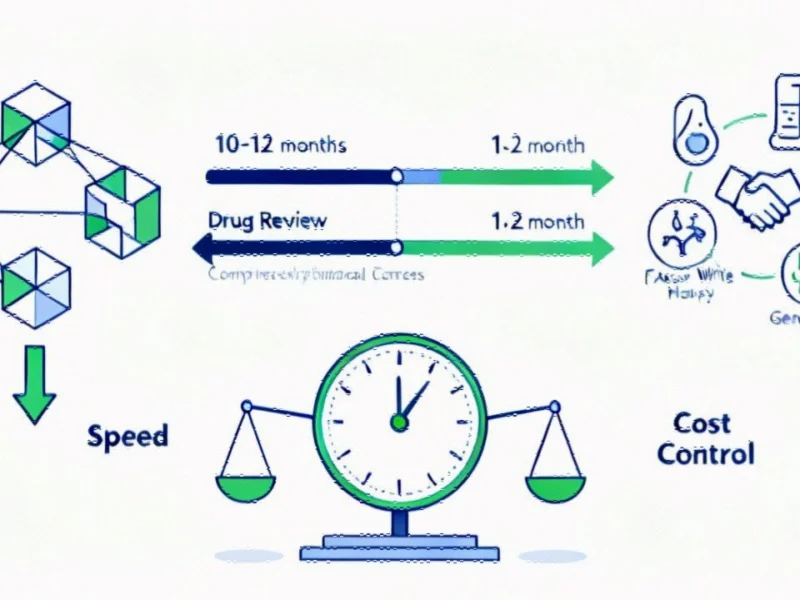
The disparity in waiting times between NHS and private facilities is substantial. Consultant orthopaedic surgeon Arpit Patel highlighted the dramatic difference: “There can be a huge discrepancy. I think at the moment in the NHS the waiting list (for orthopaedic care) is around 62 to 64 weeks. At Spire my waiting list is three months.” This gap demonstrates why the Department of Health is pursuing this strategy to address critical healthcare delays affecting thousands of patients.
Equity Concerns in Healthcare Access
Despite the potential benefits, healthcare professionals are raising important questions about equitable access. Norfolk GP Dr Clare Aitchison noted: “The problem is that at the moment patients who do find out about it (the right to choose) and therefore get access to shorter waiting lists are generally the more educated, maybe more middle class patients anyway. That is increasing health inequality again because people who have higher means are working the system better.”
This concern about creating a two-tiered access system echoes challenges seen in other sectors where market trends sometimes favor those with greater resources or information. Dr. Aitchison stressed the importance of ensuring all patients are informed about their options to prevent worsening health disparities.
Broader Implications for Healthcare Systems
The NHS-private partnership model represents a significant evolution in healthcare delivery that could influence healthcare partnerships globally. As health systems worldwide grapple with similar challenges of rising demand and limited resources, the UK’s experiment with public-private collaboration could offer valuable insights for other countries facing comparable pressures.
This approach to healthcare innovation comes at a time when other industries are also experiencing significant industry developments that reshape service delivery models. The integration of private sector efficiency with public healthcare objectives represents a delicate balancing act that requires careful monitoring and adjustment.
Technology and System Integration Challenges
Successfully implementing these healthcare partnerships requires robust technological infrastructure, a challenge that extends beyond healthcare into other sectors where recent technology implementations can sometimes encounter operational hurdles. The need for seamless data sharing between NHS and private systems adds complexity to these partnerships.
As the program expands, monitoring its impact on both waiting times and health outcomes will be crucial. The initiative represents one of several related innovations occurring across different sectors that aim to improve service delivery through strategic partnerships and technological advancement.
Future Outlook and Strategic Considerations
The long-term success of these healthcare partnerships will depend on addressing both operational efficiency and equitable access. Like other sectors experiencing transformation, healthcare must navigate complex implementation challenges similar to those faced in strategic planning across various industries.
As this model evolves, policymakers will need to carefully balance the immediate benefits of reduced waiting times against potential long-term impacts on the NHS system and healthcare equality. The ongoing evaluation of this approach will provide critical data for future healthcare delivery models both within the UK and internationally.
This article aggregates information from publicly available sources. All trademarks and copyrights belong to their respective owners.
Note: Featured image is for illustrative purposes only and does not represent any specific product, service, or entity mentioned in this article.